 Massachusetts Massachusetts
Infectious
Waste
Background Information
Definition of Infectious Medical Waste
Managing Infectious Medical Waste
Disposal of Infectious Medical Waste
OSHA Regulations
Statutes, Regulations and Guidelines
Contacts
More Information
Background Information
Medical waste differs from hazardous waste. Hazardous waste is regulated by the US EPA (and related state rules) under the Resource Conservation and Recovery Act. Medical waste is not covered federal environmental laws or US EPA regulations (with the exception of a medical waste that also meets the definition of hazardous waste). Rather, medical waste is mostly controlled by state law and associated regulations. In addition to state environmental agency laws/rules, aspects of medical waste management are also controlled by the Occupational Safety & Health Administration (federal and/or state) and Department of Transportation (federal and state).
Each of our 50 states have developed rules and implemented regulations for medical waste. The state rules vary to some extent, including terminology. Depending on which state you live in, you may hear the terms regulated medical waste, biohazardous waste or infectious medical waste. In most cases, these terms all refer to the same thing: that portion of the medical waste stream that may be contaminated by blood, body fluids or other potentially infectious materials, thus posing a significant risk of transmitting infection.
Most states have regulations covering packaging, storage, and transportation of medical waste. Some states require health care facilities to register and/or obtain a permit. State rules may also cover the development of contingency plans, on-site treatment, training, waste tracking, recordkeeping, and reporting.
In most states, the environmental protection agency is primarily responsible for developing and enforcing regulations for medical waste management and disposal. Although in some states, the department of health may play an important role or even serve as the primary regulatory agency. Where both agencies are involved, typically the department of health is responsible for on-site management and the environmental agency is responsible for transportation and disposal.
OSHA, whether it is the U.S. Department of Labor Occupational Safety & Health Administration or an OSHA state program (24 states operate their own program), regulates several aspects of medical waste, including management of sharps, requirements for containers that hold or store medical waste, labeling of medical waste bags/containers, and employee training. These standards are designed to protect healthcare workers from the risk of exposure to bloodborne pathogens. However, they also help to systematically manage wastes, which benefit the public and environment.
Regulated medical waste is defined by the US Department of Transportation as a hazardous material. DOT rules mostly apply to transporters rather than healthcare facilities; although, knowledge of these rules is important because of the liability associated with shipping waste off-site.
Definition of Infectious
Medical Waste
In Massachusetts, infectious medical waste is considered
a special solid waste. Infectious or Physically Dangerous Medical
or Biological Waste is waste, which because of its characteristics
may: cause, or significantly contribute to an increase in mortality
or an increase in serious irreversible or incapacitating reversible
illness; or pose a substantial present potential hazard to human
health or the environment when improperly treated, stored, transported,
disposed of, or otherwise managed.
The following types of waste are identified and
defined as infectious or physically dangerous medical or biological
waste:
-
Blood and Blood Products: Discarded bulk human
blood and blood products in free draining, liquid state; body fluids
contaminated with visible blood; and materials saturated/dripping
with blood;
-
Pathological Waste: Human anatomical parts, organs,
tissues and body fluids removed and discarded during surgery or
autopsy, or other medical procedures and specimens of body fluids
and their containers;
-
Cultures and Stocks of Infectious Agents and
Associated Biologicals: All discarded cultures and stocks of infectious
agents and associated biologicals, biotechnological by-product
effluents, cultures of specimens from medical and pathological
laboratories, cultures and stocks of infectious agents from research
laboratories, wastes from the production of biologicals, and discarded
live and attenuated vaccines intended for human use;
-
Contaminated Animal Carcasses, Body Parts and
Bedding: The contaminated carcasses and body parts and bedding
of all research animals known to be exposed to pathogens;
-
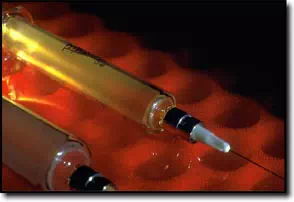
Sharps: Discarded medical articles that may cause
puncture or cuts, including but not limited to all used and discarded
hypodermic needles and syringes, pasteur pipettes, broken medical
glassware, scalpel blades, disposable razors, and suture needles;
and
-
Biotechnological By-Product Effluents: Any discarded
preparations made from genetically altered living organisms and
their products.
Managing Infectious Medical
Waste
Massachusetts’ medical
waste regulations set forth the requirements for the storage and
disposal of infectious or physically dangerous medical or biological
waste. The regulations apply to all generators of infectious or physically
dangerous medical or biological waste, except for private residences.
Generators and facilities that manage medical waste
must follow rules that are administered and enforced by the Department
of Public Health.
Storage of Infectious Medical Waste
- All medical or biological waste, except sharps, shall be contained in a primary container which is a red, fluorescent orange or orange-red plastic bag that is impervious to moisture and has sufficient strength to resist ripping, tearing, or bursting under normal conditions of use and handling, and which meets the American Society for Testing Materials (ASTM) standard D1922-06a and ASTM D1709-04. Each primary container shall:
- Be marked prominently with the universal biohazard warning symbol and the word “Biohazard” in a contrasting color; and
- Be secured so as to prevent leakage and to preclude loss of contents during handling, storage, and/or transport.
- All areas for on-site storage of containers of medical or biological waste, excluding kiosks dedicated for the sole purpose of collecting home sharps pursuant to M.G.L. c. 94C, § 27A, shall be in an uncarpeted room or area with impervious, cleanable, non-absorbent flooring, used exclusively for waste storage.
- All on-site storage areas shall:
- Have prominent signage indicating the space is used for the storage of regulated medical or biological waste;
- Be designed or equipped to prevent unauthorized access;
- Be designed or located to protect the waste from the elements and prevent access by vermin;
- Provide sufficient space to allow for clear separation of regulated medical or biological waste from any other waste, when applicable;
- Be adequate to accommodate the volume of regulated medical or biological waste generated prior to removal of waste for either waste transport off-site or on-site treatment, and
- Be maintained such that there is no putrescence of off-site odors, using refrigeration when necessary.
- Sharps shall be segregated from other wastes and aggregated immediately after use in red, fluorescent orange or orange-red leakproof, rigid, puncture-resistant, shatterproof containers that resist breaking under normal conditions of use and handling, meet ASTM standard F2132-0I, and that are marked prominently with the universal biohazard warning symbol and the word "Biohazard" in a contrasting color.
- Free draining blood and blood products and biotechnology by-product effluents shall be stored at all times in leakproof containers that are securely sealed.
- Compactors or grinders shall not be used to process medical or biological waste until it has been rendered noninfectious and safe for disposal in accordance with 105 CMR 480.150.
- All medical or biological waste, except from home sharps users, must be treated on-site or transported off-site for treatment at a minimum once per calendar year.
Disposal of Infectious
Medical Waste
-
Blood and Blood
Products
-
If the waste
generator is connected to a municipal sewerage system or septic
system, free draining blood and blood products except blood
saturated materials may be disposed of directly into these
systems unless such disposal is otherwise restricted by the
authorized approving agency.
-
If the waste
generator is prohibited by the authorized approving agency
from disposing of blood and blood products into the municipal
sewerage system or septic system, blood and blood products,
except blood saturated materials, shall be sent to an approved
incineration facility for incineration or shall be rendered
noninfectious by gas, chemical or steam sterilization prior
to disposal and disposed of in a sanitary landfill approved
by the Department of Environmental Protection or in case of
out-of-state disposal, approved by the appropriate regulatory
agency responsible for landfill approval.
-
Sharps. Containers
of sharps shall either be:
- Disposed of by incineration at an approved
incineration facility; or
-
Rendered noninfectious
as set forth in 105 CMR 480.100(F) and processed by grinding
or other effective method to eliminate the physical hazard
of the sharps and disposed of in a sanitary landfill approved
by the Department of Environmental Protection or in the case
of out-of-state disposal, approved by the appropriate regulatory
agency responsible for landfill approval.
-
Blood Saturated
Materials, Cultures and Stocks of Infectious Agents and Associated
Biologicals, Dialysis Waste and Laboratory Waste. These wastes
shall either be:
-
Biotechnology By-Product Effluents. These wastes
shall not be removed from the site of the waste generator unless
the viable organism containing recombinant DNA molecules have been
rendered noninfectious by a validated method. The following methods
shall be used as appropriate:
-
Steam sterilization;
-
Chemical disinfection;
-
Incineration
at an approved incineration facility; or
-
Other methods
approved by the Department.
- The methods, which rely on heat, shall be
evaluated mechanically and biologically by using a recording
thermometer and indicator microorganism with a defined heat susceptibility
pattern.
-
If these wastes
are rendered noninfectious by chemical disinfection, the
chemical used shall be of demonstrated efficacy against the
target or indicator organism.
-
Once rendered
noninfectious, biotechnology by-product effluents may be disposed
of directly into the waste generator's connection to the municipal
sewerage system or septic system unless such disposal is otherwise
restricted by the authorized approving agency.
-
If the generator
is prohibited by the authorized approving agency from disposing
of biotechnology by-product effluents through the municipal
sewerage system or septic system, these wastes shall be rendered
noninfectious and disposed of in a sanitary landfill approved
by the Department of Environmental Protection or in the case
of out-of-state disposal, approved by the appropriate regulatory
agency responsible for landfill approval.
-
Pathological waste
and contaminated animal carcasses shall be disposed of at
an approved incineration facility or by interment provided however
that liquid pathological waste may also be disposed in accordance
with the regulations and discarded teeth and tissue may also
be disposed of in accordance with the regulations. These wastes
shall be placed in a second three-mil bag if they are to be transported
off-site for disposal.
Labeling
Every container or
bag of waste, which has not been rendered noninfectious shall:
-
Be distinctively
marked with the international biohazard symbol and colored red
to indicate that it contains waste; and
-
In the case of sharp
wastes, be distinctively labeled to indicate that it contains sharp
waste capable of inflicting punctures or cuts.
Every container or bag
of waste which has not been rendered noninfectious and which will be
transported off the premises of the waste generator shall in addition
to the requirements of the regulations, be placed in containers which
are:
-
Rigid;
-
Leak resistant;
-
Impervious to moisture;
-
Of sufficient strength
to prevent tearing or bursting under normal conditions of use and
handling, and
-
Sealed to prevent
leakage during transport.
-
Bear a label that
states the name, address and telephone number of the generator.
The label shall be affixed in a manner that ensures that it cannot
be easily removed.
Prior to transport
for off-site disposal, waste that has been rendered noninfectious
by a method other than incineration, shall be labeled or otherwise
marked so as to clearly identify it as noninfectious medical or biological
waste and to identify the waste generator responsible for the treatment.
Such waste may be disposed of in the same manner as waste that is
not regulated, except for sharps, which shall be disposed of in accordance
with the requirements of the regulations
Policies and Procedures; Records
-
Written
policies and procedures for rendering waste noninfectious shall
be developed that assure effectiveness and compliance with the
requirements.
-
The
waste generator shall maintain records of temperature and dwell
times used in each instance where waste has been rendered noninfectious
by gas or steam sterilization and records of each biological
spore test culture result. Such records shall be retained for
at least three years.
-
The
waste generator shall maintain records of volume and type of
waste rendered noninfectious on-site which shall be available
for Department review. Such records shall be retained for at
least three years.
-
Generators shall
prepare manifests before shipping waste, which has not been rendered
noninfectious off-site. The manifest is a tracking document designed
to record the movement of waste from the generator through its
trip with a transporter to an approved disposal facility and final
disposal. The generator shall appoint a designee to prepare, sign
and maintain such manifests. The manifest must include the following
information:
- Description of waste to be shipped;
- Total quantity of waste; and
- Type of container in which waste is transported.
-
A generator shall
designate on the manifest the address of the site to which the
waste is to be delivered and sign it. The transporter of the waste
or an agent of the transporter shall sign the manifest to indicate
that the transporter has received the waste and will comply with
the generator's transportation instructions. When the waste arrives
at the approved off-site disposal facility, and has been disposed
of, the disposal facility owner or agent of the owner shall sign
the manifest and return the original to the generator.
-
If the generator
does not receive the manifest from the disposal facility within
30 days after shipment of waste by the generator, the generator
shall report this fact to the Department of Public Health.
- The generator shall maintain a copy of the manifest
both as initially sent out and as returned by the disposal facility
for a period of three years.
-
In the absence of
any restriction concerning individuals who are authorized to transport
waste, including but not limited to those imposed by boards of
health or the Department of Environmental Protection, generators
who transport their own waste shall follow the manifest requirements
set forth in the regulations.
Approval of Additional Methods of Treatment,
Storage and Disposal
The Department may approve additional methods for
the treatment, storage or disposal of infectious or physically dangerous
medical or biological waste under the following conditions: The method
has been validated through scientific studies acceptable to the Department,
and, if the waste is to be transported off-site, the waste treatment
facility has been approved by the Department of Environmental Protection,
or if the waste is to be transported out-of-state, the waste treatment
facility has been approved by the appropriate regulatory agency in
that state.
OSHA Regulations
In addition to the state medical waste environmental
regulations there are some Occupational Safety and Health Administration
(OSHA) rules that apply to medical/infectious waste. Massachusetts
is one of 26 states covered entirely by the federal OSHA program.
This program is operated by the Occupational
Safety and Health Administration. OSHA rules (Occupational
Exposure to Bloodborne Pathogens Standards) impact various aspects
of medical/infectious waste, including management of sharps, requirements
for containers that hold or store medical/infectious waste, labeling
of medical/infectious waste bags/containers, and employee training.
Statutes, Regulations
and Guidelines
Solid
Waste Management - Special Waste and Facility Requirements (310
CMR 19.000)
Contacts
Massachusetts
Department of Public Health, Division of Community Sanitation
Massachusetts
Department of Environmental Protection
More Information
Infectious
Waste Information Web Page
|

