 Wisconsin Wisconsin
Medical/Infectious
Waste
Background Information
Definition of Infectious Medical Waste
Managing Regulated Medical
Waste
OSHA Regulations
Statutes,
Regulations and Guidelines
Contacts
More Information
Background Information
Medical waste differs from hazardous waste. Hazardous waste is regulated by the US EPA (and related state rules) under the Resource Conservation and Recovery Act. Medical waste is not covered federal environmental laws or US EPA regulations (with the exception of a medical waste that also meets the definition of hazardous waste). Rather, medical waste is mostly controlled by state law and associated regulations. In addition to state environmental agency laws/rules, aspects of medical waste management are also controlled by the Occupational Safety & Health Administration (federal and/or state) and Department of Transportation (federal and state).
Each of our 50 states have developed rules and implemented regulations for medical waste. The state rules vary to some extent, including terminology. Depending on which state you live in, you may hear the terms regulated medical waste, biohazardous waste or infectious medical waste. In most cases, these terms all refer to the same thing: that portion of the medical waste stream that may be contaminated by blood, body fluids or other potentially infectious materials, thus posing a significant risk of transmitting infection.
Most states have regulations covering packaging, storage, and transportation of medical waste. Some states require health care facilities to register and/or obtain a permit. State rules may also cover the development of contingency plans, on-site treatment, training, waste tracking, recordkeeping, and reporting.
In most states, the environmental protection agency is primarily responsible for developing and enforcing regulations for medical waste management and disposal. Although in some states, the department of health may play an important role or even serve as the primary regulatory agency. Where both agencies are involved, typically the department of health is responsible for on-site management and the environmental agency is responsible for transportation and disposal.
OSHA, whether it is the U.S. Department of Labor Occupational Safety & Health Administration or an OSHA state program (24 states operate their own program), regulates several aspects of medical waste, including management of sharps, requirements for containers that hold or store medical waste, labeling of medical waste bags/containers, and employee training. These standards are designed to protect healthcare workers from the risk of exposure to bloodborne pathogens. However, they also help to systematically manage wastes, which benefit the public and environment.
Regulated medical waste is defined by the US Department of Transportation as a hazardous material. DOT rules mostly apply to transporters rather than healthcare facilities; although, knowledge of these rules is important because of the liability associated with shipping waste off-site.
Definition of Infectious Medical
Waste
The following solid wastes
are presumed to be infectious waste unless methods of testing which
are generally accepted by the medical profession demonstrate that the
waste is not infectious:
-
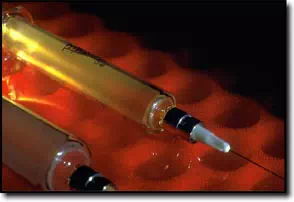
Sharps, including contaminated
sharps which are both infectious and may easily cause punctures or
cuts in the skin, including but not limited to: hypodermic needles,
syringes with needles attached, scalpel blades, lancets, broken glass
vials, broken rigid plastic vials and laboratory slides, and unused
or disinfected sharps which are being discarded, including hypodermic
needles, scalpel blades, lancets and syringes with needles attached;
- Bulk blood and body fluids from humans;
- Human tissue;
- Microbiological laboratory waste; and
- Tissue, bulk blood or body fluids from an animal,
which is carrying a zoonotic infectious agent.
Solid wastes presumed
not to be infectious wastes include the following:
-
Items soiled but not
saturated with blood or body fluids from humans included in the definition
of "bulk blood and body fluids";
-
Items soiled with body
fluids from humans not included in the definition of "bulk blood
and body fluids";
-
Intravenous tubing
after needles have been detached;
- Tissue, blood, body fluids or cultures from an animal
which is not known to be carrying or experimentally infected with a
zoonotic infectious agent;
- Animal manure and bedding;
- Other solid wastes, including but not limited to
containers, packages, waste glass, laboratory equipment and other materials
which have had no contact with blood, body fluids, clinical cultures
or infectious agents. When possible, use of these items shall be reduced,
and the items shall be reused or recycled; and
- Formerly infectious waste, after it has been treated
according to the regulations.
Managing Infectious Medical
Waste
Source separation
-
Infectious waste may
not be mixed in the same bag or waste receptacle with solid waste,
which is not infectious waste, unless mixing the wastes is necessary
to protect the health or safety of patients, employees or other persons.
- No person may separate infectious waste from solid
waste, which is not infectious waste, unless adequate measures are
taken to protect waste handlers and other persons from exposure. After
separation, solid waste previously mixed in the same bag or waste receptacle
with infectious waste shall be managed as infectious waste.
- No person may remove solid waste or infectious waste
that has been placed in a bag or waste container labeled with the biohazard
symbol, or fail to manage the waste as infectious waste from the time
of generation until the waste has been treated, unless the person follows
waste management procedures which will protect waste handlers and other
persons from exposure.
- No person may transport solid waste and infectious
waste on the same cart or vehicle unless the wastes are in separate
and identifiable bags or waste containers. If the wastes are transported
on any roads, transporter requirements apply.
Containment
No person may transport
infectious waste from the property where the waste was generated unless
the waste is put in a container which protects waste handlers and other
persons from exposure to the infectious waste and the person meets
all of the following requirements:
-
Sharps shall be contained
in rigid, punctureresistant labeled containers made of materials
including but not limited to metal or rigid plastic, designed to
prevent the loss of the contents and labeled with a visible bio hazard
emblem or with the visible words "biohazard", "sharps" or "infectious
waste".
- Infectious waste other than sharps shall be contained
according to all of the following:
- The waste shall be placed in a single plastic bag that meets
or exceeds 165 grams resistance by the ASTM method D170991 and
is tear resistant using method ASTM method D192289, or, if necessary,
a double bag that meets the same standards, or a rigid reusable
container. Copies of the testing methods are available for inspection
at Department of Natural Resources, the Secretary of State, or
the American Society for Testing and Materials.
- The bag or rigid reusable container shall be securely sealed
to prevent leakage or expulsion of the contents under normal
handling.
- Any bag containing infectious waste shall be placed in a rigid
container, including but not limited to a corrugated cardboard
container, a covered reusable container or a cart. The rigid
container shall be labeled with a visible biohazard emblem and
the word "biohazard". Bulk containers shall be small enough
to be handled by a single person.
- All reusable containers shall be disinfected after being emptied.
- No person may open a secured container of infectious
waste which is ready for transportation until immediately before treating
the waste, unless repacking is necessary to prevent spills or leakage,
or the person is conducting a waste audit or training session.
Handling
No person may handle,
load, unload, process or treat infectious wastes unless adequate measures
are taken to protect waste handlers and other persons from exposure
to the infectious wastes and unless all of the following requirements
are met:
-
All containers shall
be handled and transported to prevent the loss or spilling of the
contents.
-
Nuisance conditions
shall be prevented from developing. Appropriate measures shall be
taken to prevent odors, including but not limited to refrigerating
the infectious waste below 42 degrees Fahrenheit
until treated.
- All infectious waste shall be loaded and unloaded
by hand or by a safe mechanical method that does not damage containers
or spill their contents.
- Untreated infectious waste may not be compacted.
Storage and Transfer
No person may store infectious
wastes unless the person protects waste handlers and other persons
from exposure to the infectious waste and unless the following requirements
are met:
-
Storage includes, but
is not limited to the transfer of infectious waste. Infectious waste
generators may temporarily accumulate infectious waste in individual
containers near the place where the waste was generated, prior to
moving the waste to an onsite infectious waste storage facility.
- No person may operate or maintain an infectious
waste storage facility unless the person has obtained an operating
license for storing solid waste and the storage facility meets all
the requirements for handling and storing infectious waste.
Infectious waste storage
facilities that which meet any of the following conditions are exempt
from the requirement to obtain an operating license and preparing a
plan of operation, but shall meet the minimum operating requirements
for storing infectious waste:
-
Storage facilities
that are located on the property where the infectious waste is generated.
-
Storage facilities
which are located on the property where the infectious waste is generated
and which accept infectious waste from offsite generators, if the
total quantity of infectious waste, including items mixed with infectious
waste, accepted from offsite is less than the quantity generated
onsite or less than 500 pounds per month, whichever is less and
if the waste is accepted on a notforprofit and costonly basis.
-
Sharps collection stations
which comply with all requirements.
- Storage facilities for infectious waste, which is
also, is hazardous waste, provided that the storage facility is regulated.
Plan of Operation
No person may establish
or construct an infectious waste storage facility or expand an existing
facility unless the person has obtained a plan of operation approval
from the department or unless the facility is exempt from licensing
requirement.
Minimum Requirements for the Storage of Infectious
Waste
No person may operate
or maintain an infectious waste storage facility unless the storage
area meets all of the following requirements:
Requirements for Sharps Collection Stations
No person may operate
or maintain a sharps collection station unless the person complies
with all of the following requirements:
Transportation and Shipping
No person may transport
or ship infectious waste in Wisconsin unless adequate measures are
taken to protect waste handlers, the public and the environment from
exposure to the infectious waste, and all of the following requirements
are met:
Minimum Requirements for Transporting Infectious
Waste
No person may transport infectious waste unless all
of the following minimum requirements are met:
The person shall transport
the infectious waste only to licensed solid waste facilities that store
or treat infectious waste, or exempt from licensing or other requirements.
Other transportation regulations, such as federal department of transportation
standards, may also apply.
Operating Requirements for Licensed Infectious
Waste Transporters
Infectious waste transporters
that are required to be licensed shall comply with all the following
requirements, in addition to other applicable rules:
Licensed infectious waste
transporters shall notify the department in writing of all significant
changes in service, including adding or replacing a vehicle, changing
the destination to which the infectious waste is hauled, expanding
the service area into another county, or terminating service.
Treatment Methods
No person may dispose
of infectious waste in a solid waste disposal facility unless the infectious
waste has undergone treatment that effectively renders the waste noninfectious.
The treatment method shall be chosen by considering the properties
of the waste being treated and the degree of microbial contamination.
The treatment method
may also need to comply with air standards for control of hazardous
pollutants, and with state or federal regulations for wastewater and
occupational health and safety. All infectious waste shall be treated
by one or more of the following infectious waste treatment methods:
-
Incineration;
- Steam disinfection;
- Chemical disinfection;
- Mechanical grinding and chemical disinfection;
- Mechanical grinding and heat disinfection;
- Gas disinfection; and
- Other treatment methods and processes that render
the waste noninfectious and shall be appropriate with respect to all
of the following: the properties of the waste being disinfected, the
manufacturer's recommended use of the disinfectant, the cleanliness
of the surface of the waste, the contact time, the physical properties
of the waste, the concentration of the disinfectant and the degree
of microbial contamination.
The following infectious
wastes must be treated as follows:
-
Human tissue shall
be treated by methods which render the tissue both noninfectious
and unrecognizable as human tissue, or incineration, where the tissue
is transformed into an ash which would not be recognized as being
from a human being.
-
Animal tissue known
to be carrying or experimentally infected with a zoonotic infectious
agent shall be treated by methods which render the tissue noninfectious,
incineration, burial on the land on which the animal was kept, or
rendering or other methods which incorporate the animal into a consumer
product in accordance with all other applicable state and federal
regulations. Note: For animals and animal waste
used in HIV and HbV research, refer to OSHA bloodborne pathogen
standard.
-
Sharps shall be treated
by a method which both renders the sharp noninfectious and renders
the sharp broken and not able to be reused, such as by a grinding
or shredding process, or incineration.
-
Bulk blood shall be
treated by biological treatment in an approved or permitted municipal
or industrial wastewater treatment facility (bulk blood may be transported
to the wastewater treatment facility through the sewer system), methods
which render the blood noninfectious, or incineration.
-
Body fluids and bloodcontaminated
urine and feces shall be treated by any approved methods or by disposal
in a septic system.
Treatment Facilities
No person may operate
or maintain an infectious waste treatment facility unless they have
obtained an operating license as a solid waste processing facility
and the facility meets all applicable requirements for containing,
handling, storing and treating infectious waste.
Records and Infectious Waste Manifests
All infectious waste
generators shall keep records of the amount of infectious waste sent
offsite for treatment. Records may consist of any of the following:
copies of infectious waste manifests, invoices or records received
from the infectious waste treatment facility, logs or other written
documentation of the amount of infectious waste sent offsite for treatment.
These records shall be kept for at least 3 years after they were created.
If the 3year period expires during an unresolved enforcement action,
the period is automatically extended until resolution of the pending
enforcement action.
No person may store,
transfer, transport or treat infectious waste beyond the property where
the waste was generated unless the waste is accompanied by an infectious
waste manifest. The infectious waste manifest may either be a Wisconsin
infectious waste manifest form supplied by the department or an alternative
manifest form.
After an infectious waste
manifest has been initiated, all persons who store, transfer, transport
or treat the waste shall sign the infectious waste manifest form provided
by the DNR, even if the infectious waste generator is exempt from manifesting,
and shall deliver the infectious waste manifest form to the next person
who handles the waste.
The following persons
are exempt from record keeping and manifest requirements:
The following persons
are exempt from the requirements to use infectious waste manifests,
but shall follow the requirement for keeping records:
-
An infectious waste
generator transporting infectious waste only on private roads on
the same property where the infectious waste was generated and using
vehicles owned or leased by the infectious waste generator or by
one of the generators in the group.
-
An infectious waste
generator transporting less than 50 pounds per calendar month of
untreated infectious waste away from the property where the waste
was initially generated, including items which are mixed with the
infectious waste.
-
Infectious waste generators
located on the same property who manage their infectious waste together
and who, as a group, transport less than 50 pounds per calendar month
of untreated infectious waste away from the property.
The infectious waste
manifest form shall include all of the following information:
-
The
place of origin of the infectious waste, including the name, address,
telephone number, and name of contact person and type of facility
where the infectious waste was generated, including but not limited
to: hospitals, clinics, nursing homes, sharps collection stations
and other facilities.
- The route for the infectious waste, including
the name, address, telephone number, license number and name of contact
person for any and all persons storing, transporting or treating
the infectious waste beyond the location where the infectious waste
was generated.
- The destination for disposal of the treated
infectious waste, including the name, address, telephone number,
solid waste disposal facility license number and name of a contact
person.
- The composition of the infectious waste, including
the type or types of infectious waste.
- The quantity of the infectious waste, including
both the number of containers and the total weight, whether known
or estimated, of infectious waste including waste which is mixed
with the infectious waste.
- The signature of an authorized representative
of each facility or licensed transporter handling the waste from
generation through treatment.
Retention of Infectious Waste Manifests and
Related Records
Infectious waste manifests
and related records shall be retained as follows:
-
The infectious waste
generator shall retain the original infectious waste manifest, and
the certification of infectious waste treatment for at least 3 years
after the waste has been treated, and provide the department copies
of manifests upon request. If the 3year period expires during an
unresolved enforcement action, the period is automatically extended
until resolution of the pending enforcement action. Note: Hospitals,
clinics and nursing homes should keep records for at least 5 years.
-
Each licensed infectious
waste transporter and each owner or operator of a storage or transfer
facility, combustor, incinerator or infectious waste treatment facility
which handles or disinfects infectious waste shall retain a copy
of each manifest for at least 3 years.
Infectious Waste Annual Reports
An infectious waste generator
who is either required to use manifests under or to submit progress
reports on medical waste reduction shall submit an annual report to
the department on a form supplied by the department and the annual
filing fee for the report
Infectious waste generators
who manifest infectious waste as a group may choose to submit a single
annual report on behalf of the group and which is signed by a representative
of each generator in the group.
Except as required, the
annual report shall be submitted by March 1 foractivities performed
during the preceding calendar year. The annual report shall contain
the information on the department's form and shall be signed by the
administrator or chief executive officer of the infectious waste generator.
Medical Waste Reduction Plan
Unless exempt, medical
facilities are required to prepare a medical waste reduction plan and
implement policies which will do all of the following:
-
Reduce the amount of
medical waste generated by medical facilities;
-
Prevent the mixing
of infectious waste with non-infectious waste;
-
Promote practical alternatives
to disposable items in medical facilities; and
-
Maintain effective
waste reduction programs.
The medical waste generator
must ensure the medical waste reduction plan is prepared property,
annually assess the plan and results annually, update the plan at least
every 5 years, and keep a copy of the current plan and have it available
for DNR review upon request.
The plan must include
training of employees in waste management policies, practices and procedures
for medical and other wastes generated, and an audit of the medical
facility's current solid waste management practices.
OSHA
Regulations
In addition to the state medical waste environmental
regulations there are some Occupational Safety and Health Administration
(OSHA) rules that apply to medical/infectious waste. Wisconsin
is one of 26 states covered entirely by the federal OSHA program. This
program is operated by the Occupational
Safety and Health Administration. OSHA rules (Occupational Exposure
to Bloodborne Pathogens Standards) impact various aspects of medical/infectious
waste, including management of sharps, requirements for containers
that hold or store medical/infectious waste, labeling of medical/infectious
waste bags/containers, and employee training.
Statutes, Regulations and
Guidelines
Wisconsin
Administrative Codes Pertaining to Medical and Infectious Waste
Contacts
Wisconsin Department
of Natural Resources
More Information
Wisconsin DNR - Waste Management
Program Medical/Infectious Waste
|
|

